Frequently Asked Questions
General Questions
Category III CPT codes
- are temporary and for new or emerging services, so some payers do not adopt them while others impose their own definitions and interpretations.
- signify only that there is some evidence of clinical efficacy and of “evolving clinical utilization”
Category I CPT codes
- are permanent
- signify that
- the clinical efficacy of the services has been documented in research that meets rigorous AMA standards
- The services are performed by many physicians or other qualified healthcare professionals and are consistent with current medical practice
- Other benefits of Category I codes
- More uniform and consistent adherence to the descriptors as approved by the CPT Editorial Panel
- Fewer denials of coverage for ABA services on the false premise that they are “experimental,” “unproven,” or “not medically necessary.”
- More uniform and consistent adherence to the descriptors as approved by the CPT Editorial Panel
- No add-on codes
- All codes are uniform time increments – 15 minutes per unit
- Concurrent billing with certain code pairs is clearly denoted in educational materials
- Social skills code has been replaced with group treatment codes
- Family training with QHP is “with or without patient present”
- Assessment codes have been streamlined and clarified. 97151 is for initial and reassessment by QHP. Supporting assessments may follow.
- “Exposure” codes have been revamped and clarified to specify that they are for functional analysis and treatment of destructive behavior, respectively (but they remain Category III).
Yes. Under HIPAA, if a payer accepts electronic claims submissions, they must utilize Category I CPT codes.
No. Payers have their own procedures and timelines for implementing new codes, so providers must obtain that information from each payer with whom they work.
In 2013, the American Medical Association (AMA) established a definition for a qualified healthcare professional (QHP), in terms of which providers may report medical services: “A ‘physician or other qualified health care professional’ is an individual who is qualified by education, training, licensure/regulation (when applicable) and facility privileging (when applicable) who performs a professional service within his/her scope of practice and independently reports that professional service.”
Possible QHPs for the 2019 CPT codes for adaptive behavior services, depending on state licensure laws, health insurance regulations, Centers for Medicare & Medicaid Services’ (CMS) and/or other payers’ policies:
- Licensed Behavior Analysts
- Board Certified Behavior Analysts, Board Certified Behavior Analysts-Doctoral
- Other licensed professionals who have behavior analysis in their profession’s scope of practice and their individual scope of competence
With time based codes a CPT code may be reported when half the time increment outlined in the code descriptor has been met. In the case of the 2019 Adaptive Behavior codes, work lasting 8-22 minutes is reportable as one unit; work lasting less than 8 minutes is not reportable.
- Alert your payers about the new codes!
- Use the code-conversion table and other resources from our website to work with payers to achieve consistent use of the 2019 code set.
- If you haven’t already, give payers CASP’s ASD treatment guidelines and APBA’s white paper on identifying ABA interventions.
- Obtain accurate MUEs for the new codes.
- Review your contracts.
- Calculate the value of your services. Have meaningful data on the full cost of providing a service (e.g., cost of staff compensation packages including benefits, liability insurance, malpractice insurance, practice expenses such as equipment, reinforcers, technology, data collection software, EMRs) to discuss with payers.
- Negotiate! As a party to your contract you always have the ability to request a review of contract terms with you payers. This includes reevaluation of reimbursement rates and payer policies and procedures related to your agreement. Be sure that any requests for renegotiation comply with your contract terms regarding submission format and notice criteria/timelines.
No. The new codes will be carrier priced for 2019. That means that payers will establish reimbursement rates for each code with providers via the contract negotiation process.
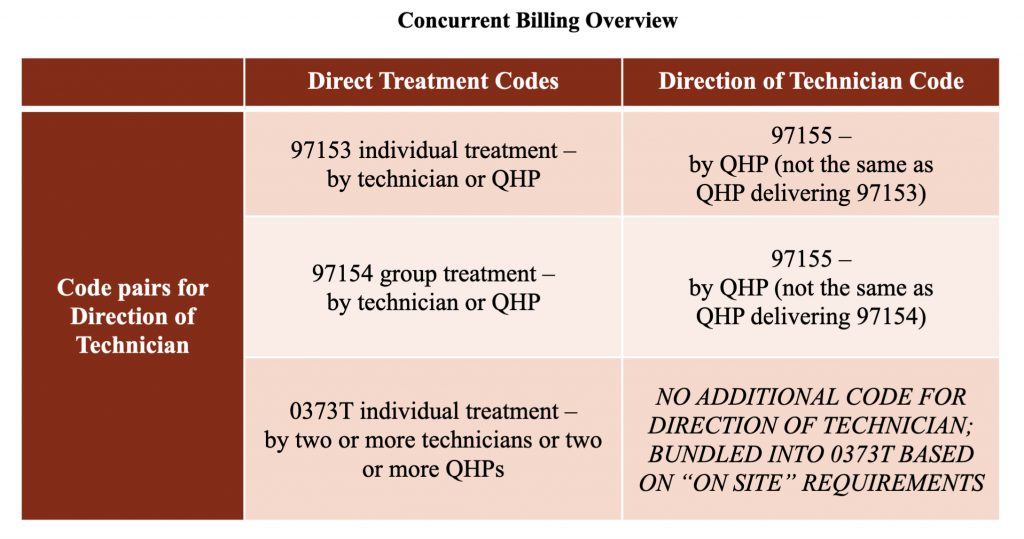
See the table below (click to enlarge).
There is no separate code for those indirect services in the new CPT code set (nor was there in the Category III CPT code set). Some payers may supplement the adaptive behavior services code set with a HCPCS or other CPT code (e.g., H0032, G9012, H2019) to report indirect activities. In the event payers do not, the activities that occur prior to and after the face-to-face time should be bundled so that reimbursement for those codes captures both face-to-face and non-face-to-face time.
No. Code 97155 should be reported only for services where the QHP is either engaged directly with the patient or is directing a technician in implementing a modified protocol with the patient.
No. That is an indirect service for which CPT does not allow stand-alone codes. Some payers may allow the use of HCPCS or other CPT codes to report that work.
This varies based on state law and payer policy. Review your contracts and provider manuals for guidance on whether telehealth is approved by your individual payers.
No. Payers may supplement the 2019 CPT codes with HCPCS or other CPT codes for indirect services or other activities, which would be specified in your modified 2019 contracts.
The 2019 CPT® Code Book and the CPT® Assistant article both contain information that is essential for a full understanding of the code set and how it should be reported. Those materials are copyrighted by the AMA, so we cannot distribute them without express permission from the AMA.
“Direction” in the context of code 97155 refers to the QHP directly monitoring the delivery of treatment to a patient by a behavior technician. The focus is on ensuring that treatment protocols are implemented correctly in order to maximize benefit to that patient. Direction of a technician includes, but is not limited to, the QHP frequently observing the technician implementing the patient’s protocols with the patient, providing instructions and confirming or corrective feedback as needed, and/or demonstrating correct implementation of a new or modified treatment protocol with the patient while the technician observes, followed by the technician implementing the protocol with the patient while the QHP observes and provides feedback. That service should be reported and billed using code 97155 (adaptive behavior treatment with protocol modification administered by physician or other qualified health care professional). The technician’s time is separately reportable under 97153 (adaptive behavior treatment by protocol administered by technician under the direction of a physician or other qualified health care professional). Time reported and billed must be face-to-face time with the patient.
“Supervision” of a technician or other employee by a QHP generally refers to processes through which the QHP ensures that the supervisee (a) practices in a competent, professional, and ethical manner in accordance with the standards of the profession; (b) engages with and follows the employer’s policies and procedures; (c) continues to develop their knowledge and skills; and (d) receives the personal support needed to cope with the stressors and demands of their position. “Supervision” may also involve activities to enable the supervisor and supervisee to comply with specific requirements for obtaining or maintaining a paraprofessional or professional credential, such as a certification or license, or to fulfill ethical responsibilities. Supervision activities that do not involve delivery of services directly to patients are generally not reportable or billable to health plans using CPT codes, though some payers may allow them to be billed using HCPCS or other codes. Those that do involve direct delivery of services to maximize benefits to individual patients may be reportable and billable to a health plan and fulfill some supervision requirements for certification or licensure purposes, but only the former should be reported to the health plan.
Note: The Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Managers (2nd ed.) use the terms “case supervision” and “clinical direction” to refer to the work conducted by the QHP to develop, deliver, and oversee implementation of a patient’s treatment plan. Those terms encompass both direct contact with the patient or caregivers and indirect services. Direct adaptive behavior services by the QHP include delivering assessment or treatment face-to-face with the patient (reported with codes 97151, 97153 with modifier, 97155, 0362T, 0373T, 97158) or caregiver(s) (reported with codes 97156, 97157). Only code 97151 allows non-face-to-face activities (reviewing records, scoring assessments, and preparing a treatment plan or progress report) to also be reported and billed. Indirect services by the QHP include activities involved in ongoing monitoring of patient progress and revising protocols, preparing for assessment or treatment sessions by the QHP and/or technicians, reviewing data, and writing progress notes – that is, activities like those described in the “prior” and “after” sections of the clinical examples in this document. As indicated in the introduction, there is no stand-alone CPT code for those indirect services, so they must be bundled with direct services for payment unless the payer allows them to be reported and billed with a HCPCS or other code.
No. Modifying written protocols and other indirect activities (writing session notes, updating treatment goals or plans, reviewing data, creating materials, etc.) are not billable with any CPT code in the current adaptive behavior/ABA services code set except 97151, which allows the behavior analyst to bill for direct as well as some indirect services (e.g., reviewing records, interviewing the patient or caregivers, scoring assessments) to develop an initial treatment plan or a progress report. For all other codes in the set, only the time spent face-to-face with a patient or caregiver is billable. “Face-to-face” means that the provider is actively engaging the patient or caregiver in assessment or treatment. Simply having them nearby while completing indirect work does not fulfill the CPT face-to-face requirement. The Coalition understands that a great deal of indirect work is required to deliver ABA services effectively and ethically. In fact, the authors of the current CPT code set advocated for the American Medical Association’s CPT Editorial Panel to issue a standalone code for indirect services, but they declined to do so. It is important to note that indirect services are “bundled” with direct services for the vast majority of CPT codes that are used by medical and other professionals; it is not specific or unique to the ABA code set. That said, the Coalition advocates for payers to allow ABA providers to use a HCPCS or CPT code to bill for indirect services, which some payers are doing. For information about activities that constitute billable protocol modification activities for CPT codes 97155, 97158, and 0373T, indirect services associated with each CPT code, and bundling direct and indirect services for billing, please see the Supplemental Guidance Article on our Resources webpage.
No. It is certainly desirable for ABA provider organizations to have systems and procedures in place to ensure that patients receive high-quality care. Those may include having experienced professional behavior analysts perform quality assurance activities, such as reviewing treatment plans or protocols drafted by newly licensed or certified behavior analysts or providing staff with general supervision and training to enhance their job performance or professional development. Such activities are considered indirect, however, because they do not involve face-to-face, active engagement of patients or their caregivers in assessment or treatment services. Therefore, quality assurance and other administrative activities performed by behavior analysts are not billable to health plans unless that is specified clearly in payer policies and contracts. The only indirect services that are billable to health plans with current CPT codes are those encompassed in the descriptor for CPT code 97151 (behavior identification assessment administered by the qualified health care professional), i.e., “non-face-to-face analyzing past data, scoring/interpreting the assessment, and preparing the report/treatment plan.” For additional information about direct (face-to-face, billable) and indirect (non-face-to-face, non-billable) services, please see FAQs on related topics and the Supplemental Guidance Article under Resources on this website.
Code-Specific Questions
97151
Assessments and reassessments require extensive non-face-to-face time for the QHP to score assessments, review records and data, and write or update the treatment plan. That can take several hours, and in many cases occurs across multiple dates of service. That is why only this code allows for reporting of non-face-to-face time.
No. This code is intended for reporting initial assessment and treatment plan development and reassessment and progress reporting by the QHP (timeframes for reassessments are determined by payer policy or medical necessity). 97151 includes face-to-face time with the patient and/or caregivers to conduct assessments as well as non-face-to-face time for reviewing records, scoring and interpreting assessments, and writing the treatment plan or progress report. The QHP must have conducted both the face-to-face and non-face-to-face activities to report this service. Day-to-day assessment and treatment planning by the QHP are bundled into the treatment codes below (i.e., 97153-97158 and 0373T); therefore, 97151 cannot be used to report those indirect services because they do not meet all requirements of the code descriptor.
No. It is certainly desirable for ABA provider organizations to have systems and procedures in place to ensure that patients receive high-quality care. Those may include having experienced professional behavior analysts perform quality assurance activities, such as reviewing treatment plans or protocols drafted by newly licensed or certified behavior analysts or providing staff with general supervision and training to enhance their job performance or professional development. Such activities are considered indirect, however, because they do not involve face-to-face, active engagement of patients or their caregivers in assessment or treatment services. Therefore, quality assurance and other administrative activities performed by behavior analysts are not billable to health plans unless that is specified clearly in payer policies and contracts. The only indirect services that are billable to health plans with current CPT codes are those encompassed in the descriptor for CPT code 97151 (behavior identification assessment administered by the qualified health care professional), i.e., “non-face-to-face analyzing past data, scoring/interpreting the assessment, and preparing the report/treatment plan.” For additional information about direct (face-to-face, billable) and indirect (non-face-to-face, non-billable) services, please see FAQs on related topics and the Supplemental Guidance Article under Resources on this website.
97152
No. This code is for reporting supplemental assessments conducted by the technician that the QHP determines are needed to develop the treatment plan or progress report (see code 97151). Additionally, as indicated in the clinical example, the QHP reviews the assessment procedures with the technician and has the technician practice recording data. That may occur on the day of an assessment session with a patient or several days leading up to the session(s). That work by the QHP is bundled into the value of code 97152 and is not reported separately.
0362T
As indicated in the article about the 2019 adaptive behavior/ABA services CPT codes in the November 2018 issue of the American Medical Association CPT® Assistant newsletter, destructive behaviors include but are not limited to “… self-injurious behavior, aggression, property destruction, pica, elopement, and other behaviors associated with high-risk medical consequences or property damage” (p. 4). That encompasses any behaviors that jeopardize a patient’s health or safety and for which research documents that ABA services are effective for preventing or reducing the risk of medical consequences, i.e., injuries and/or health problems. Examples in addition to those just listed include but are not limited to feeding difficulties, sleep difficulties, rumination, bruxism, mouthing objects, inadequate fluid intake, skin picking, resistance to or lack of cooperation with dental and medical care procedures, and other behaviors that may result in the need for medical treatment. CPT codes 0362T and 0373T are appropriate for reporting ABA assessment and treatment of such behaviors if all required elements of those codes are met (QHP/behavior analyst on site, two or more technicians, environment customized to patient’s behavior).
On site is defined as the QHP being “immediately available and interruptible.” This means that the QHP is at the same site and can join the session if needed.
For codes 0362T and 0373T, the term “customized” means that the environment is configured to safely conduct a functional analysis of destructive behavior (0362T) or treatment for that behavior (0373T). For some patients, this can be accomplished in the home. For example, in the case of a patient who displays aggression using objects, those objects that the patient might use as dangerous weapons (e.g., a wooden baseball bat) would be removed and replaced with soft items (e.g., a foam baseball bat). Other patients may require treatment in a padded treatment room. For example, a patient with severe head banging may require functional analysis and initial treatment in a padded treatment room because the behavior causes tissue damage and places the patient at risk for detached retinas.
No. These services should be preauthorized for cases where all four of the criteria in the code descriptor are met.
In order to be truly available to assist behavior technicians who are rendering 0362T or 0373T, the QHP cannot be providing direct assessment or treatment services to another client or a caregiver at the same time, because they cannot immediately leave their session(s) whenever needed to assist with the other session(s). The QHP could, however, be “immediately available and interruptible” to assist with 0362T or 0373T services if they are providing direction to a behavior technician who is implementing intervention with a client, reported with code 97155 (adaptive behavior treatment with protocol modification, administered by QHP, which may include simultaneous direction of technician). When scheduling 0362T and 0373T sessions, providers must ensure that a QHP will be present in the same location and not assigned to deliver any direct services to clients or caregivers that would prevent them from being “immediately available and interruptible.”
97153
If no protocols have been modified and a QHP is simply acting in place of the technician, report 97153 with a modifier to indicate the higher-level service provider.
Yes, as long as the criteria in the descriptors of both codes are met. A single QHP may not report 97153 and 97155 concurrently. See the Concurrent Billing Overview table in the Other Frequently Asked Questions section.
97154
No. 97158 is intended to be reported for QHP-led group sessions only.
Yes, as long as the criteria in the descriptors for both codes are met. A single QHP may not report 97154 and 97155 concurrently.
A group includes at least 2 patients but no more than 8.
Yes. Report the applicable code for each patient attending the group session.
97155
In two cases: (1) When a QHP conducts 1:1 direct treatment with the patient to observe changes in behavior or troubleshoot treatment protocols; or (2) when the QHP joins the patient and the technician during a treatment session to direct the technician in implementing a new or modified treatment protocol. In the second case, 97153 should be reported concurrently (see Concurrent Billing Overview in the Other Frequently Asked Questions section).
An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing a specified service to address a patient’s assessment or treatment goal(s) and (b) implementation of the procedures with the patient.
Adaptive behavior service protocol modification involves changes made by a qualified health care provider (QHP) to the procedures for implementing an adaptive behavior service. Protocol modification includes but is not limited to (a) adjustments to specific components of a protocol (e.g., treatment targets, treatment goals, observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative stimuli, contextual variables); (b) observations to determine if the protocol components are functioning effectively for the patient or require adjustments; (c) active direction of a technician while the technician delivers a service to a patient to ensure that the procedures are being implemented correctly, to correct errors in implementation, or to train the technician to implement a modified protocol; and (d) QHP implementation of the protocol with the patient to determine if changes are needed to improve patient progress or to test a modified protocol. Any protocol-modification services that are delivered during face-to-face sessions with patients or caregivers are billable. Modifying written protocols is an indirect service that is not reported separately, but is bundled with 97155, 97158 or 0373T for payment.
97156
Yes. Those are separate and distinct services delivered to different family members by different providers.
This is determined by payer policy. Immediate family members are almost always covered, but some payers may have a broader definition and include others such as babysitters, teachers, day care providers, etc.
97157
No. Report this code for each set of caregivers for a given patient who attend the group session. For example, if five sets of parents attend the group session, report the code once for each set.
97158
No. 97158 is intended to be reported for QHP-led group sessions only.
A group includes at least 2 patients but no more than 8.
Yes. Report the applicable code for each patient attending the group session.
Adaptive behavior service protocol modification involves changes made by a qualified health care provider (QHP) to the procedures for implementing an adaptive behavior service. Protocol modification includes but is not limited to (a) adjustments to specific components of a protocol (e.g., treatment targets, treatment goals, observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative stimuli, contextual variables); (b) observations to determine if the protocol components are functioning effectively for the patient or require adjustments; (c) active direction of a technician while the technician delivers a service to a patient to ensure that the procedures are being implemented correctly, to correct errors in implementation, or to train the technician to implement a modified protocol; and (d) QHP implementation of the protocol with the patient to determine if changes are needed to improve patient progress or to test a modified protocol. Any protocol-modification services that are delivered during face-to-face sessions with patients or caregivers are billable. Modifying written protocols is an indirect service that is not reported separately, but is bundled with 97155, 97158 or 0373T for payment.
An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing a specified service to address a patient’s assessment or treatment goal(s) and (b) implementation of the procedures with the patient.
No. Code 97158 is intended to be used any time a behavior analyst leads a treatment session with 2 – 8 patients. Although protocol modification MAY occur during such a session, that is not required. See the FAQ about protocol modification for a description of protocol modification activities that are and are not billable.
0373T
As indicated in the article about the 2019 adaptive behavior/ABA services CPT codes in the November 2018 issue of the American Medical Association CPT® Assistant newsletter, destructive behaviors include but are not limited to “… self-injurious behavior, aggression, property destruction, pica, elopement, and other behaviors associated with high-risk medical consequences or property damage” (p. 4). That encompasses any behaviors that jeopardize a patient’s health or safety and for which research documents that ABA services are effective for preventing or reducing the risk of medical consequences, i.e., injuries and/or health problems. Examples in addition to those just listed include but are not limited to feeding difficulties, sleep difficulties, rumination, bruxism, mouthing objects, inadequate fluid intake, skin picking, resistance to or lack of cooperation with dental and medical care procedures, and other behaviors that may result in the need for medical treatment. CPT codes 0362T and 0373T are appropriate for reporting ABA assessment and treatment of such behaviors if all required elements of those codes are met (QHP/behavior analyst on site, two or more technicians, environment customized to patient’s behavior).
No. Report only the total time of one technician. Example: if three technicians are needed for a 3-hour session, report 12 units of 0373T (15 minutes x 12 units = 180 minutes, or 3 hours).
No. That and other indirect services must be bundled with this code.
On site is defined as the QHP being “immediately available and interruptible.” This means that the QHP is at the same site and can join the session if needed.
For codes 0362T and 0373T, the term “customized” means that the environment is configured to safely conduct a functional analysis of destructive behavior (0362T) or treatment for that behavior (0373T). For some patients, this can be accomplished in the home. For example, in the case of a patient who displays aggression using objects, those objects that the patient might use as dangerous weapons (e.g., a wooden baseball bat) would be removed and replaced with soft items (e.g., a foam baseball bat). Other patients may require treatment in a padded treatment room. For example, a patient with severe head banging may require functional analysis and initial treatment in a padded treatment room because the behavior causes tissue damage and places the patient at risk for detached retinas.
An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing a specified service to address a patient’s assessment or treatment goal(s) and (b) implementation of the procedures with the patient.
Adaptive behavior service protocol modification involves changes made by a qualified health care provider (QHP) to the procedures for implementing an adaptive behavior service. Protocol modification includes but is not limited to (a) adjustments to specific components of a protocol (e.g., treatment targets, treatment goals, observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative stimuli, contextual variables); (b) observations to determine if the protocol components are functioning effectively for the patient or require adjustments; (c) active direction of a technician while the technician delivers a service to a patient to ensure that the procedures are being implemented correctly, to correct errors in implementation, or to train the technician to implement a modified protocol; and (d) QHP implementation of the protocol with the patient to determine if changes are needed to improve patient progress or to test a modified protocol. Any protocol-modification services that are delivered during face-to-face sessions with patients or caregivers are billable. Modifying written protocols is an indirect service that is not reported separately, but is bundled with 97155, 97158 or 0373T for payment.
In order to be truly available to assist behavior technicians who are rendering 0362T or 0373T, the QHP cannot be providing direct assessment or treatment services to another client or a caregiver at the same time, because they cannot immediately leave their session(s) whenever needed to assist with the other session(s). The QHP could, however, be “immediately available and interruptible” to assist with 0362T or 0373T services if they are providing direction to a behavior technician who is implementing intervention with a client, reported with code 97155 (adaptive behavior treatment with protocol modification, administered by QHP, which may include simultaneous direction of technician). When scheduling 0362T and 0373T sessions, providers must ensure that a QHP will be present in the same location and not assigned to deliver any direct services to clients or caregivers that would prevent them from being “immediately available and interruptible.”

